
Of those, 29 percent completed living wills, 33 percent filed health care proxies and 32 percent remained "undefined," meaning the type of advance directive wasn't specified or was combined. Of nearly 800,000 people, 37 percent completed some kind of advance directive. People with chronic illnesses were only slightly more likely than healthy individuals to put their wishes down on paper.įor the analysis, published in the July issue of Health Affairs, researchers reviewed 150 studies published between 20 that looked at the proportion of adults who completed advance directives. adults have them, according to a recent study. Even though advance directives have been promoted by health professionals for nearly 50 years, only about a third of U.S.

Attention to the family’s emotional responses is appropriate and appreciated.Not everyone is so motivated to tackle these issues.
Throughout the interview, there are usually a number of opportunities to respond to feelings and to support family members. Seek verbal confirmation of understanding and agreement. Especially if not choosing aggressive care, assure the family of the attention to patient comfort and dignity that will occur. If your recommendation differs from the family’s, let them know, and seek clarification of the differences.Īfter such a discussion and negotiation, restate or reframe the value statement that best matches the patient’s expressed or implied values.ĭiscuss specific procedures and directives, as appropriate.ĭepending on the family’s substituted judgment, describe what will and will not be done.
END OF LIFE DECISIONS DOCUMENT PROFESSIONAL
Use such statements and recommendations to support family’s impressions or to provide a professional observation upon which the family can build. Share your interpretation of the meaning of the patient’s words and behaviors. If no specific statements or directives had been given, try to recreate a values history at least on the issue of survival versus comfort and dignity.īe an active participant. If so, reinforce the principle of substituted judgment following the patient’s previously stated preferences. Question whether the patient has ever communicated clear procedural directives or a values history. Try to achieve a consensus about the patient’s clinical situation, especially prognosis. What is each person’s relationship with the patient? How is each person responding to the patient’s present condition?Ĭlarify the difference between substituted judgment and decisions in the best interest of the patient. Sit down, and establish rapport with each person present. Try to keep those who know the patient best in the center of decision making.įind a quiet place to meet where each family member can be seated comfortably. If neither durable power-of-attorney nor written directive is in effect, determine who should be approached to make the decisions. If durable power-of-attorney or a living will is present, these documents should guide the subsequent process as much as possible.
END OF LIFE DECISIONS DOCUMENT FULL
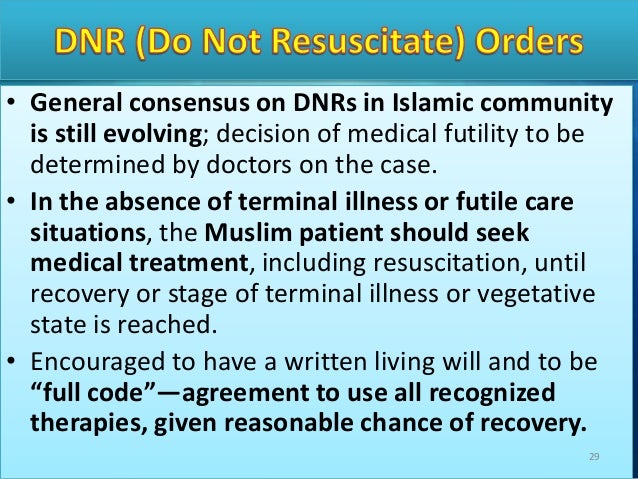
The most common pitfalls in establishing plans of care for patients who lack decision-making capacity include failure to reach a shared appreciation of the patient’s condition and prognosis failure to apply the principle of substituted judgment offering the choice between care and no care, rather than offering the choice between prolonging life and quality of life too literal an interpretation of an isolated, out-of-context, patient statement made earlier in life and failure to address the full range of end-of-life decisions from do-not-resuscitate orders to exclusive palliative care. Communication and decision making in these situations require a complex integration of relevant conceptual knowledge of ethical implications, the principle of surrogate decision making, and legal considerations and communication skills that address the highly charged emotional issues under discussion. Because advance directives are not yet the norm, end-of-life decisions for patients without medical decision-making capacity are made regularly within discussions between the patient’s physician and family.


 0 kommentar(er)
0 kommentar(er)
